1. What are the major risk factors for heart disease?
The
major risk factors for heart disease are smoking, high cholesterol
levels, high blood pressure, physical inactivity, obesity, diabetes,
age, gender, and heredity (including race).
See
also on this site: Heart Disease Risk Factors
2.
What is high blood pressure and how is it treated?
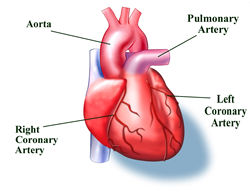
Your
heart pumps blood through a network of arteries, veins, and capillaries.
The moving blood pushes against the arterial walls, and this force
is measured as blood pressure.
High
blood pressure results from the tightening of very small arteries
(arterioles) that regulate the blood flow through your body. As
these arterioles tighten (or constrict), your heart has to work
harder to pump blood through the smaller space, and the pressure
inside the vessels grows.
High
blood pressure is so dangerous because it often has no symptoms.
High blood pressure tends to run in families. Men are at higher
risk than women, and blacks are at greater risk than whites.
In
most cases, high blood pressure can be controlled by eating a
low-fat and/or low-salt diet; losing weight, if necessary; beginning
a regular exercise program; learning to manage stress; quitting
smoking; and drinking alcohol in moderation, if at all. Medicines,
called antihypertensives, are available if these changes do not
help control your blood pressure within 3 to 6 months.
See
also on this site: High Blood Pressure (Hypertension)
3.
What is cholesterol and why is it so important?
Cholesterol
is a fat-like substance (lipid) found in all body cells. Your
liver makes all of the cholesterol your body needs to form cell
membranes and make certain hormones. Extra cholesterol enters
your body when you eat foods that come from animals (meats, eggs,
and dairy products). Although we often blame the cholesterol found
in foods that we eat for raising blood cholesterol, the main culprit
is saturated fat, which is also found in our food. So, we should
limit foods high in cholesterol or saturated fat. Foods rich in
saturated fat include butter fat in milk products, fat from red
meat, and tropical oils such as coconut oil.
Cholesterol
travels to cells through the bloodstream in special carriers called
lipoproteins. Two of the most important lipoproteins are low-density
lipoprotein (LDL) and high-density lipoprotein (HDL). Doctors
look at how LDL and HDL relate to each other and to total cholesterol.
LDL
particles deliver cholesterol to your cells. LDL cholesterol is
often called "bad cholesterol" because high levels are
thought to lead to the development of heart disease. Too much
LDL in the blood causes plaque to form on artery walls, which
starts a disease process called atherosclerosis. When plaque builds
up in the coronary arteries that supply blood to the heart, you
are at greater risk for having a heart attack.
HDL
particles carry cholesterol from your cells back to your liver,
where it can be eliminated from your body. HDL is known as "good
cholesterol" because high levels are thought to lower your
risk for heart disease.
See
also on this site: Cholesterol
4.
What are triglycerides?
Triglycerides
are fats that provide energy for your muscles. Like cholesterol,
they are delivered to your body's cells by lipoproteins in the
blood. If you eat foods with a lot of saturated fat or carbohydrates,
you will raise your triglyceride levels. Elevated levels are thought
to lead to a greater risk for heart disease, but scientists do
not agree that high triglycerides alone are a risk factor for
heart disease.
Although
triglycerides serve as a source of energy for your body, very
high levels can lead to diabetes, pancreatitis, and chronic kidney
disease. As triglyceride levels rise, HDL levels fall, which may
help explain why people with high triglycerides appear to have
an increased risk for heart disease.
See
also on this site: Cholesterol
5.
What is atherosclerosis?
Atherosclerosis
is a condition where a waxy substance forms inside the arteries
that supply blood to your heart. This substance, called plaque,
is made of cholesterol, fatty compounds, calcium, and fibrin (a
blood-clotting material). Scientists think atherosclerosis begins
when the very inner lining of the artery (the endothelium) is
damaged. High blood pressure, high levels of cholesterol, fat,
and triglycerides in the blood, and smoking are believed to lead
to the development of plaque.
Atherosclerosis
may continue for years without causing symptoms.
See
also on this site: Coronary Artery Disease
6.
What is coronary bypass surgery?
Bypass
surgery improves the blood flow to the heart with a new route,
or "bypass," around a section of clogged or diseased
artery.
The
surgery involves sewing a section of vein or artery from the leg
or chest (called a graft) to bypass a part of the diseased coronary
artery. This creates a new route for blood to flow, so that the
heart muscle will get the oxygen-rich blood it needs to work properly.
Coronary
bypass surgery has proved safe and effective for many patients
who have the procedure. You can expect to stay in the hospital
for about a week after surgery, including at least 1 to 3 days
in the Intensive Care Unit (ICU). Your doctor may also recommend
that you participate in a cardiac rehabilitation program. These
programs are designed to help you make lifestyle changes like
starting a new diet and exercise program, quitting smoking, and
learning to deal with stress.
See
also on this site: Coronary Bypass Surgery
7.
Besides coronary bypass surgery, what other treatment options
are available to a patient with narrowed or blocked arteries?
A
severely narrowed coronary artery may need treatment to reduce
the risk of a heart attack. Coronary bypass surgery is one form
of treatment, but there are other therapies that have been found
effective among carefully selected patients.
Angioplasty,
which opens narrowed arteries, is performed by interventional
cardiologists. They use a small balloon-tipped catheter that they
inflate at the blockage site to flatten the plaque against the
artery wall. A thin wire is inserted into an artery in the leg
and is guided to the site of narrowing in the coronary artery.
The catheter is slipped over this guidewire and positioned at
the blockage, where the balloon is inflated. After treatment,
the wire, catheter, and balloon are removed. The hospital stay
and recovery time for this procedure are shorter than that of
bypass. But, about 35% of patients are at risk for more blockages
in the treated area (called restenosis). If restenosis is going
to occur, it will usually happen within 6 months of the procedure.
A
stent procedure is used in conjunction with balloon angioplasty.
It involves implanting a mesh-like metal device into an artery
at a site narrowed by plaque. The stent is mounted on a balloon-tipped
catheter, threaded through an artery, and positioned at the blockage.
The balloon is then inflated, opening the stent. Then, the catheter
and deflated balloon are removed. The opened stent keeps the vessel
open and stops the artery from collapsing. Restenosis rates are
generally around 15-20%.
Atherectomy
may be an option for certain patients who cannot have balloon
angioplasty. A high-speed drill on the tip of a catheter is used
to shave plaque from artery walls.
Laser
ablation uses a catheter that has a metal or fiberoptic probe
on the tip. The laser uses light to "burn" away plaque
and open the vessel enough so that a balloon can further widen
the opening.
Percutaneous
transmyocardial revascularization (PTMR) is performed by a cardiologist
in the cardiac catheterization laboratory. Using local anesthesia,
the cardiologist inserts a long, thin tube (called a catheter)
in an artery in the leg that leads to the heart. A laser is then
fed through the catheter and used to create tiny holes in the
heart muscle. These holes become channels for blood to flow to
oxygen-starved areas of the heart. Researchers believe that the
procedure may cause new vessels to form, reducing the pain of
angina. PTMR is currently being used on patients who have not
responded to other treatments such as medicines, angioplasty,
or coronary artery bypass surgery.
See
also on this site: Coronary Artery Disease
8.
What is arrhythmia?
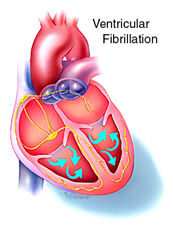
Arrhythmias
are irregular heartbeats caused by a disturbance in the electrical
activity that paces your heartbeat. Arrhythmias cause nearly 340,000
deaths each year. Almost everyone's heart skips a beat at one
time or another. These mild, one-time palpitations are harmless.
But there are more than 4.3 million Americans who have recurrent
arrhythmias, and these people should be under the care of a doctor.
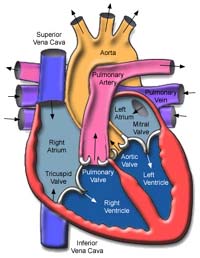
Arrhythmias
can be divided into two categories: ventricular and supraventricular.
Ventricular arrhythmias happen in the heart's two lower chambers,
called the ventricles. Supraventricular arrhythmias happen in
the structures above the ventricles, mainly the atria, which are
the heart's two upper chambers.
Arrhythmias
are further defined by the speed of the heartbeats. A very slow
heart rate, called bradycardia, means the heart rate is less than
60 beats per minute. Tachycardia is a very fast heart rate, meaning
the heart beats faster than 100 beats per minute.
See
also on this site: Arrhythmia
9.
What is atrial fibrillation?
Atrial
fibrillation is a fast, irregular rhythm where single muscle fibers
in your heart's upper chambers twitch or contract. According to
the American Heart Association (AHA), atrial fibrillation is a
major cause of stroke, especially among older people. This irregular
rhythm may cause blood to pool in the heart's upper chambers.
The pooled blood can lead to clumps of blood called blood clots.
A stroke can occur if a blood clot travels from the heart and
blocks a smaller artery in the brain (a cerebral artery).
See
also on this site: Categories of Arrhythmia
10.
What is a pacemaker and how does it work?
A
pacemaker is a surgically implanted device that helps to regulate
your heartbeat. Pacemakers use batteries to produce electrical
impulses that make the heart pump. The impulses flow through tiny
wires (called leads) that are attached to the heart. The impulses
are timed to flow at regular intervals.
Most
pacemakers work only when they are needed. These are called demand
pacemakers. They have a sensing device that either shuts off the
pacemaker if the heartbeat is above a certain rate or turns the
pacemaker on when the heart is beating too slowly.
Pacemaker
batteries can last up to five years or longer. Pacemakers and
batteries can be replaced during a minor surgical procedure.
See
also on this site: Pacemakers
11.
What is mitral valve prolapse?
The
mitral valve regulates the flow of blood from the upper-left chamber
(the left atrium) to the lower-left chamber (the left ventricle).
Mitral valve prolapse (MVP) means that one or both of the valve
flaps (called cusps or leaflets) are enlarged, and the flaps'
supporting muscles are too long. Instead of closing evenly, one
or both of the flaps collapse or bulge into the atrium. MVP is
often called click-murmur syndrome because when the valve does
not close properly, it makes a clicking sound and then a murmur.
MVP
is one of the most common forms of valve disease. It happens more
often in women and tends to run in families. Most of the time,
MVP is not a serious condition. Some patients say they feel palpitations
(like their hearts skip a beat) or sharp chest pain. If you have
MVP, you should talk to your doctor about taking antibiotic medicine
before dental procedures or general surgery, especially if you
have mitral regurgitation or thickened valve leaflets. This medicine
will prevent infection of the valve.
See
also on this site: Mitral Valve Prolapse
12.
What is congestive heart failure?
Heart
failure means your heart is not pumping as well as it should to
deliver oxygen-rich blood to your body's cells.
Congestive
heart failure (CHF) happens when the heart's weak pumping action
causes a buildup of fluid (called congestion) in your lungs and
other body tissues. CHF usually develops slowly. You may go for
years without symptoms, and the symptoms tend to get worse with
time. This slow onset and progression of CHF is caused by your
heart's own efforts to deal with its gradual weakening. Your heart
tries to make up for this weakening by enlarging and by forcing
itself to pump faster to move more blood through your body.
Many
therapies can help to ease the workload of your heart. Treatment
options include lifestyle changes, medicines, transcatheter interventions,
and surgery.
See
also on this site: Congestive Heart Failure
13.
What does the term "enlarged heart" mean?
An
enlarged heart means the heart is larger than normal due to heredity,
or disorders and diseases such as obesity, high blood pressure,
and viral illnesses. Sometimes doctors do not know what makes
the heart enlarge.
See
also on this site: Dilated Cardiomyopathy
14.
What is cardiac catheterization?
Cardiac
catheterization is the method doctors use to perform many tests
available for diagnosing and for treating coronary artery disease.
Cardiac catheterization is used with other tests such as angiography
and electrophysiology studies (EPS).
The
method involves threading a long, thin tube (called a catheter)
through an artery or vein in the leg or arm and into the heart.
Depending on the type of test your doctor has ordered, different
things may happen during cardiac catheterization. For example,
a dye may be injected through the catheter to see the heart and
its arteries (a test called angiography), or electrical impulses
may be sent through the catheter to study irregular heartbeats
(tests called electrophysiology studies).
See
also on this site: Cardiac Catheterization
15.
What is a thallium stress test?
A
stress test is a common test that doctors use to diagnose coronary
artery disease. The test helps doctors see how the heart is working.
A thallium stress test is a nuclear study in which a radioactive
substance is injected into your bloodstream to show how blood
flows through your arteries. Doctors can see if parts of the heart
muscle are damaged or dead, or if there is a serious narrowing
in an artery.
See
also on this site: Nuclear (Thallium) Stress Test
16.
What is an EPS?
Electrophysiology
(EPS) studies use cardiac catheterization techniques to study
patients who have irregular heartbeats (called arrhythmias). EPS
shows how the heart reacts to controlled electrical signals. These
signals can help doctors find out where in the heart the arrhythmia
starts and what medicines will work to stop it. EPS can also help
doctors know what other catheter techniques could be used to stop
the arrhythmia.
EPS
uses electrical signals to help doctors find out what kind of
arrhythmia you have and what can be done to prevent or control
it. Doctors will perform a cardiac catheterization procedure in
which a long, thin tube (called a catheter) will be put into an
artery in your leg and threaded into your heart. This catheter
can be used to send the electrical signals into your heart. Stimulating
the heart will cause an arrhythmia, and doctors can record where
in the heart it started. In some cases, you might be given a medicine
to cause an arrhythmia. Certain medicines can also be given through
the catheter to see which ones will stop the arrhythmia.
See
also on this site: Electrophysiology (EPS) Studies
17.
What is the difference between a "beta blocker" and
a "clot buster?"
A
beta blocker is a medicine that limits the activity of a hormone
called epinephrine. Epinephrine increases blood pressure and heart
rate. So, beta blockers work by limiting the activity of epinephrine,
which, in turn, lowers your blood pressure and decreases your
heart rate.
Clot
busters are thrombolytic agents that may be given if you are having
a heart attack or an ischemic stroke (a stroke caused by a blood
clot). The term thrombolysis means to dissolve a clot, and that
is exactly what these medicines do. In some cases, these medicines
can dissolve a clot within minutes.
Clot
busters work best when given right away. Some studies have shown
that the medicines may offer little benefit if they are given
more than a few hours after the first symptoms of a heart attack
or ischemic stroke.
See
also on this site: Medicines for Cardiovascular Disease
18.
What is carotid artery disease?
Carotid
artery disease is a form of disease that affects the vessels leading
to the head and brain (cerebrovascular disease). Like the heart,
the brain's cells need a constant supply of oxygen-rich blood.
This blood supply is delivered to the brain by the 2 large carotid
arteries in the front of your neck. If these arteries become clogged
or blocked, you can have a stroke.
Carotid
artery disease is usually caused by atherosclerosis, which is
a hardening and narrowing of the arteries. As we age, fat deposits,
cholesterol, calcium, and other materials build up on the inner
walls of the arteries. This build-up forms a wax-like substance
called plaque. As the plaque builds up, the arteries become narrower,
and the flow of blood through the arteries becomes slower.
Lifestyle
changes, medicines, transcatheter interventions, or surgery can
be used to treat carotid artery disease and lower your risk of
a stroke.
See
also on this site: Carotid Artery Disease
19.
What is an aneurysm and how is it treated?
An
aneurysm is a balloon-like bulge in a blood vessel that can affect
any large vessel in your body. An aneurysm happens when the pressure
of blood passing through part of a weak blood vessel forces the
vessel to bulge outward, forming what you might think of as a
thin-skinned blister. Not all aneurysms are life threatening,
but those found in the arteries in our bodies often need to be
treated. If the bulging stretches the artery too far, this vessel
may burst, causing a person to bleed to death.
Aneurysms
can occur in blood vessels anywhere in the body. They usually
form in the brain or in the aorta (the main artery carrying blood
from the heart). In many cases, aneurysms are associated with
other types of cardiovascular disease, especially high blood pressure
and atherosclerosis. Traumatic injuries, infections, and congenital
conditions can also lead to an aneurysm.
Treatment
depends on the size and location of your aneurysm and your overall
health. Aneurysms in the upper chest (ascending aorta) are usually
operated on right away. Aneurysms in the lower chest or the area
below your stomach (descending thoracic and abdominal portions
of the aorta) may not be as life-threatening. Aneurysms in these
locations are watched regularly. If they become about 5 cm (almost
2 inches) in diameter, continue to grow, or begin to cause symptoms,
your doctor may want you to have surgery to stop the aneurysm
from bursting.
Doctors
also may prescribe medicine, especially medicine that lowers blood
pressure (such as a beta blocker), to relieve the stress on the
arterial walls. Medicine to lower blood pressure is especially
useful for patients where the risk of surgery may be greater than
the risk of the aneurysm itself.
Cardiologists
at the Texas Heart Institute have been using a nonsurgical technique
to treat high-risk patients with aortic aneurysms. This technique
is useful for patients who cannot have surgery because their overall
health would make it too dangerous. The procedure uses a balloon-tipped
catheter to insert a spring-like device called a stent at the
site of the aneurysm. The balloon is inflated to open up the stent,
and once the catheter and deflated balloon are removed from the
artery, the stent acts as a barrier between the blood and the
arterial wall. The blood flows through the stent, decreasing the
pressure on the wall of the weakened artery. This decrease in
pressure can prevent the aneurysm from bursting.
See
also on this site: Aneurysms
20.
What is a stroke and what are the warning signs of stroke?
A
stroke is an injury to the brain that may also severely affect
the body. A stroke happens when blood supply to part of the brain
is cut off or when there is bleeding into or around the brain.
This can happen if a blood clot blocks an artery in the brain
or neck or if a weakened artery bursts in the brain.
Risk
factors for stroke include high blood pressure, smoking, heart
disease, diabetes, and a high red blood cell count. The risk of
stroke also increases with age. Heavy alcohol use increases your
risk of bleeding (hemorrhagic) strokes.
The
warning signs for stroke may include a sudden, temporary weakness
or numbness in your face or in your arm or leg; trouble talking
or understanding others who are talking; temporary loss of eyesight,
especially in one eye; double vision; unexplained headaches or
a change in headache pattern; temporary dizziness or staggering
when walking; or a transient ischemic attack (TIA).